When Precision Met Urgency
Managing a Recurrent Brain Hemorrhage
Dr Mukesh N. Sharma
Director, Neurointerventional & Stroke
Mr. OTS, a 50-year-old gentleman with a complex medical background including diabetes mellitus on regular treatment, chronic liver disease with portal hypertension, and a history of carcinoma of the sigmoid colon status post left hemicolectomy (June 2025), presented following a fall at home in Rajasthan. He developed decreased responsiveness, headache, and sluggish tongue movements and was initially managed at a local hospital before being referred to Marengo CIMS Hospital on 7th January 2026 for advanced neurological care.
Clinical evaluation and imaging revealed a recurrent left frontal intracranial hemorrhage with subarachnoid extension, raising concern for an underlying vascular etiology. His medical history also included a previous left frontal lobe intracranial hemorrhage in July 2025, placing him at a significantly high risk for re-bleeding. Despite the complexity of his condition, he remained vitally stable on admission.
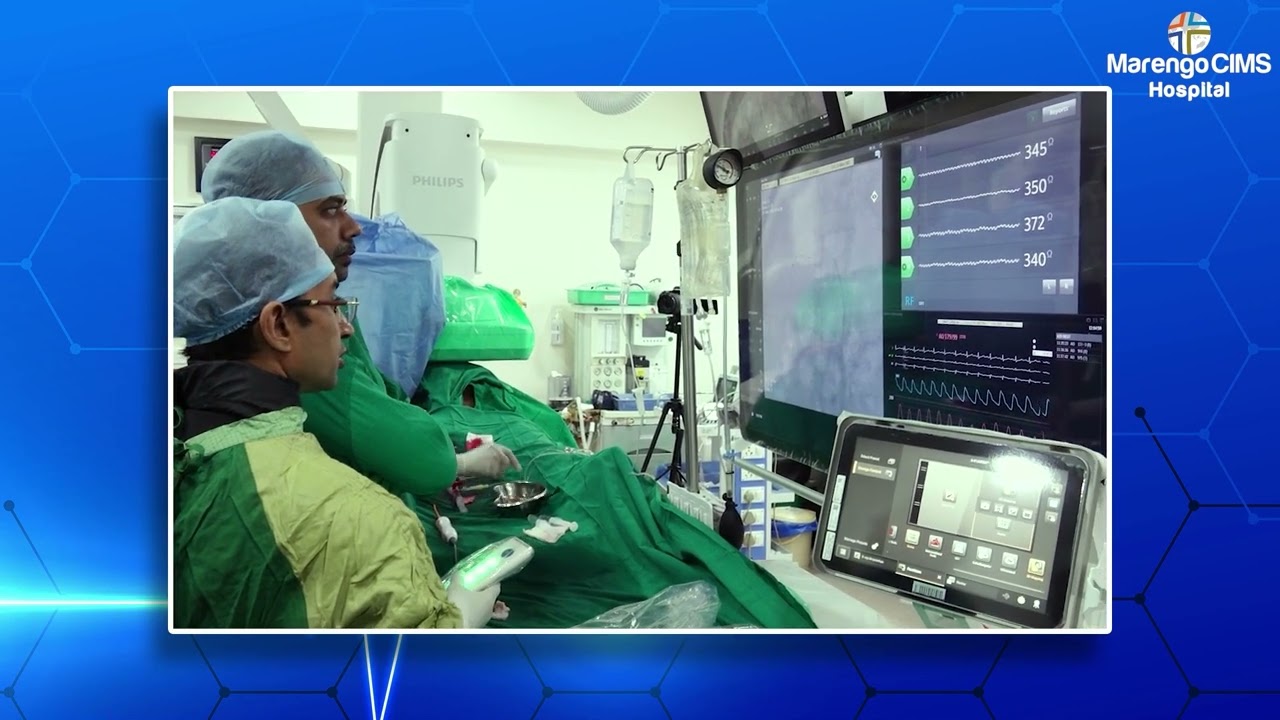
A multidisciplinary team led by Dr. Keval Changadiya (Neurology), with gastroenterology input from Dr. Bhavesh Thakkar, planned definitive management. Digital Subtraction Angiography (DSA) performed by Dr. Mukesh N. Sharma confirmed a small arteriovenous malformation (AVM) supplied by middle frontal branches of the pericallosal and callosomarginal arteries. In view of recurrent cortical bleed, endovascular treatment was deemed essential to prevent further hemorrhage. Successful AVM embolization was carried out on 8th January 2026.
Post-procedure, the patient was closely monitored in the ICU and later shifted to the ward, showing an uneventful and steady recovery. By 10th January 2026, Mr. OTS was discharged in stable hemodynamic condition with appropriate medical management, dietary advice, and a planned follow-up after 15 days—highlighting how timely DSA-guided intervention can be life-saving in unexplained cortical brain bleeds and effective in preventing re-bleeding.
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0